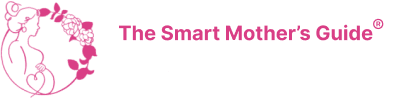
Some of you aren’t going to like what I’m about to say,
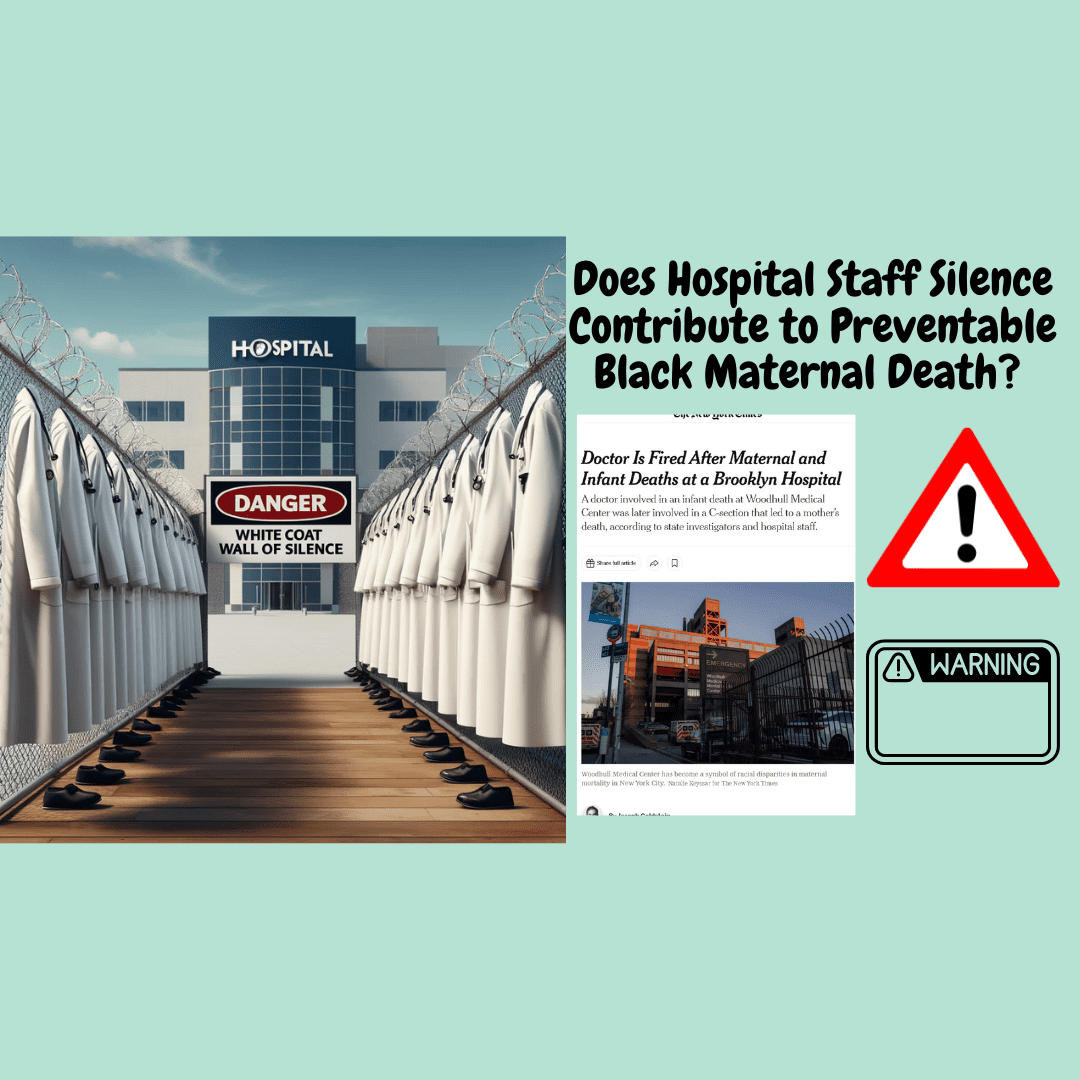
The successful birth (via VBAC) of Olympian Allyson Felix, performed by an
We have lost another mother. A Black mother. Her husband lost a
Abnormal vaginal bleeding warrants immediate attention, and proper clinical management. The two
While some significant employers now offer doula coverage, including Walmart and Microsoft,
American Heart Month brings awareness about our heart health, especially for pregnant

Traveling during the holiday season can be stressful but here are some